

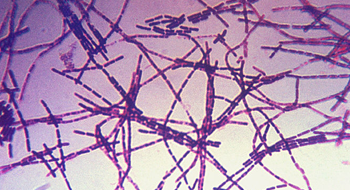

Anthrax is a serious zoonotic disease, which means it can infect humans and animals, caused by the bacteria Bacillus anthracis. Natural outbreaks occur in cows, sheep, deer, zebras and other grazing animals. As these animals graze, they may ingest dormant B. anthracis spores from the soil. The elevated temperature and CO2 levels inside an animal help activate the dormant spore, which then enters the toxin-producing, vegetative (growth) stage in its life cycle. Humans who contact or consume infected animals or animal products, such as wool or hides, are at risk of contracting anthrax. Different doses, infection routes and bacterial strains all affect the mortality rate of B. anthracis. Even with treatment, inhalation anthrax can be 50% lethal, while cutaneous anthrax is rarely deadly with treatment.
B. anthracis is considered an effective bioterrorism agent for a number of reasons, including its ability to be effectively aerosolized and grown in large industrial quantities, its high fatality rate when aerosolized, and the persistence of its spores in the environment – which can survive for decades. Spores finely ground to < 5 micons remain aerosolized for long periods of time and can lodge deep within an individual’s lungs, causing inhalation anthrax.
Virulence factors are what make an organism dangerous. Dormant B. anthracis spores activate in a host body and multiply, releasing three proteins, the Protective Antigen (PA), Edema Factor (EF), and Lethal Factor (LF). The protective antigen binds to host cells, allowing the other two protein toxins to enter and kill the cells. The edema and lethal factors interfere with normal cell signaling and water balance, causing the cells to cease function, swell and die. Loss of the genes required for the expression of these three proteins (located on the pXO1 plasmid) result in a non-virulent strain. Inside a host organism, many B. anthracis cells are engulfed by macrophages, cells of the immune system, which try to lyse (kill), the bacteria. B. anthracis cells avoid this host defense by producing a protective capsule that prevents lysis. Loss of the genes required for capsule production (located on the pXO2 plasmid) also result in a non-virulent strain.
Symptoms depend on the type of anthrax contracted - cutaneous (skin), gastrointestinal, or inhalation.
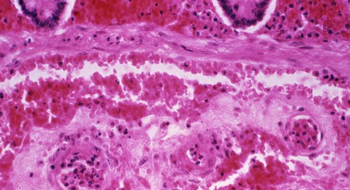
Cutaneous (skin) anthrax accounts for 95% of all cases and is rarely fatal if treated. It occurs when B. anthracis spores infect previous cuts or lesions in the skin. Symptoms appear within 1-5 days of exposure, beginning with an itchy red bump that eventually ruptures and develops into a usually painless black sore, called an eschar, which falls off in 2-3 weeks. In addition, patients usually have flu-like symptoms and often have edema, or swelling, around the infection site.
Gastrointestinal anthrax occurs after eating contaminated food, such as improperly cooked meat, and after 2-5 days causes food poisoning-like symptoms, including severe abdominal pain, vomiting and fever. It can be up to 50% fatal.
Inhalation anthrax is the most deadly form of anthrax. Symptoms normally appear within a week of exposure, but may not appear for 2 months. This incubation period depends on the amount of anthrax spores the victim was exposed to and the health of the infected individual. Symptoms begin with mild respiratory symptoms that quickly develop into severe respiratory distress (breathing difficulties), shock, and death if not treated. Fatality is 100% without treatment, and was 45% with treatment in the 2001 inhalation anthrax cases.
Generally, anthrax should be treated with a course of antibiotics, such as ciprofloxacin, as soon as exposure is suspected. If treated promptly with antibiotics, patients are likely to overcome the infection with few complications. Patients with delayed antibiotic treatment typically do not fare as well because antibiotics only inhibit bacterial growth, they do not neutralize the deadly toxins already present. This is why early disease identification and treatment is important to stop bacterial growth and toxin accumulation.
The anthrax vaccine is currently only available to those who are at high risk of B. anthracis exposure, such as laboratory or military personnel. Public vaccines are not available for several reasons; they have not been tested in all age groups; the current vaccine has a relatively high risk of side effects; and the long course of vaccine treatment – 6 initial vaccine shoots spread over 18 months and annual boosters for those at higher risk. There is only one FDA licensed anthrax vaccine, the Anthrax Vaccine Adsorbed (AVA). This vaccine contains three of the proteins required for virulence (PA, EF and LF). The immune system mainly develops antibodies against the Protective Antigen (PA), thus called because vaccination with this protein alone is enough to protect individuals from anthrax.
Dembek, Z.F. [Senior Editor]. (2007). Anthrax, Chapter 4, Medical Aspects of Chemical and Biological Warfare. Publisher: Department of Defense, Office of The Surgeon General, US Army, Borden Institute. 2007: 672 p.; ill http://www.bordeninstitute.army.mil/published_volumes/biological_warfare/biological.html
Inglesby, T.V., et al. Anthrax as a Biological Weapon, 2002: Updated Recommendations for Management. JAMA. 2002; Vol 287, No. 17: 2236-2252.
Ascenzi, P., et al. Anthrax Toxin: A Tripartite lethal combination. Federation of European Biochemical Societies Letters. 2002. Vol 531: 384-388.