
The "Spanish" flu pandemic of 1918 and 1919 caused the deaths of 20-50 million people worldwide including up to 675,000 in the U.S. While only about 1% of those infected with the virus died, it became one of the deadliest viruses ever known to man. The 1918 flu has been described as capable of sickening and killing a person on the same day. The virus is an H1N1 type A influenza. Symptoms of infection were similar to, but more severe than typical, seasonal flu. Viral pneumonia leading to acute respiratory distress was the primary cause of death. Recently, the virus was reconstituted from frozen tissue samples from a woman who died from the virus.
Although it is not known where the 1918 flu virus began infecting humans and transmitting from person-to-person, the U.S. experienced its first wave of illness in the spring of 1918. It was dubbed the “Spanish” flu because Spanish newspapers published many reports of the pandemic while publications from nations involved in the World War I refrained. Some scientists think the “Spanish” flu designation might have been in error because of reports of it cropping up outside of the region before it affected the Spanish population. It is still unclear where the virus and the pandemic originated.
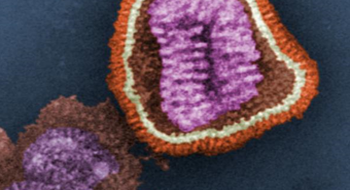
When the 1918 flu disappeared, no samples of the virus were retained for scientific study. In 1997, however, scientists recovered fragments of the virus’s RNA genome from the preserved remains of infected people. The genome of the flu virus is composed of 8 RNA segments. Recently, scientists were able to remake 1918 flu using a technique called reverse genetics. They started by making DNA copies of the virus genome segments because DNA is easier to manipulate in the lab than RNA. Each of those copies was then placed into a larger piece of circular DNA called a plasmid. Those eight DNA circles are then put into an animal cell. The animal cell produces the proteins that correspond to the 8 segments which then form the flu virus. The technique also allows scientists to selectively manipulate individual parts of the virus when doing experiments.
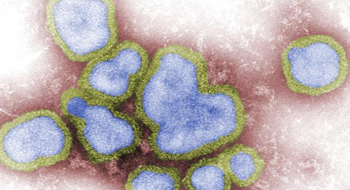
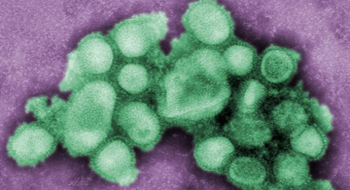
Flu strains are named for the H and N proteins, hemagglutinin and neuraminidase, which stick out from the surface of the virus like spikes. These protein spikes allow influenza to infect and damage cells and are what the immune system recognizes. The hemagglutinin spike allows the virus to bind to and enter cells. After co-opting the cells molecular machinery to produce more viruses, the neuraminidase spike is used to escape the cell, destroying it in the process. The 1918 influenza is an H1N1 strain and research on the reconstituted virus shows that it was particularly infective and had the unusual property of being able to infect mice, which typical human influenza strains cannot.
During the 1918 pandemic doctors did not have vaccines, antivirals, or antibiotics to treat or prevent infections and associated complications. Since then, four drugs have been developed to fight influenza infections; amantadine, rimantadine, oseltamivir (Tamiflu) and zanamivir (Relenza). Tamiflu and amantadine have both been shown to be effective against engineered viruses containing the parts of the 1918 flu and vaccines have also protected mice against viruses with some of the 1918 influenza components. However, it is still unclear whether drugs or vaccines would be effective against the fully reconstituted 1918 influenza virus. Currently, the U.S. only has 2.5 million doses of Tamiflu in its stockpile, raising concerns that we have not adequately prepared for a potential pandemic caused by avian H5N1 influenza.
WHO, CDC, NIAID, NIH, HHS