Avian influenza virus, strain H5N1, is the latest flu virus with the potential to trigger a pandemic outbreak of flu due to its high lethality in birds and humans. The human population has no known natural immunity to H5N1 because it is genetically distinct from the three flu strains currently circulating in humans (H1N1, H1N2, and H3N2). Bird disease and death from H5N1 have occurred throughout Asia where close interaction between people and poultry have resulted in 114 human cases and 59 deaths from late Dec. 2003 to Sept. 19, 2005 according to WHO. Hundreds of millions of farm birds have been killed throughout Asia in an attempt to control the spread of the virus. New influenza strains like H5N1 arise when two different viruses infect the same animal such as a bird or pig. Since influenza has a segmented RNA genome, individual segments can be exchanged between viruses in a single infected cell creating a new virus. This rare event is called a genetic shift.
Further changes to the virus in the form of mutations result because influenza virus has no ability to proofread its genome as it replicates. These subtle changes to the characteristics of a strain are collectively called genetic drift and are seen in flu viruses every season. This is precisely why the flu vaccine must be updated every year.
Currently, humans are thought to contract H5N1 through close contact with infected poultry or surfaces contaminated by feces and body fluids from infected birds. Although consistent and effective person-to-person transmission has not occurred, a probable transmission involved a mother caring for her sick child. Should genetic drift result in an increased ability to transmit the virus from person-to-person, infection is expected to occur through inhalation of expelled viruses or contact with contaminated surfaces, similar to current seasonal flu outbreaks. fight the infections. However, the virus was able to cross the ocean with troops arriving to fight in Europe during World War I. Foreign troops soon became exposed to the virus and carried it back to their home countries starting new waves of infection.
H5N1 is now common in the bird population of many Asian countries. The close proximity of birds, humans, and other animals susceptible to H5N1 and human flu strains are ideal for the genetic exchange needed to increase transmission.
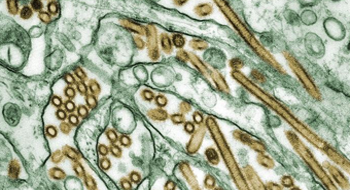
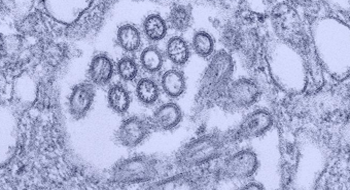
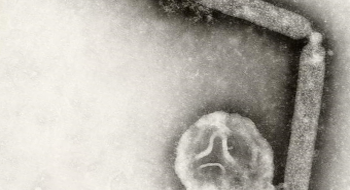
Flu strains are named for the H and N proteins, hemagglutinin and neuraminidase, which stick out from the surface of the virus like spikes. These protein spikes allow influenza to infect and damage cells and are what the immune system recognizes. The hemagglutinin spike allows the virus to bind to and enter cells. After co-opting the cells molecular machinery to produce more virus, the neuraminidase spike is used to escape the cell, destroying it in the process.
Antiviral drugs like Tamiflu and Relenza inhibit the production of neuraminidase in infected cells, preventing viral escape and reducing illness severity. Many countries are stockpiling Tamiflu from its sole producer, Roche Laboratories, to prepare for a pandemic flu. The U.S. stockpile contains enough Tamiflu to treat only 2.3 million adults and 100,000 children. Two other companies are currently developing vaccines, which are currently being tested in clinical trials. The efficacy of the vaccine against H5N1 in humans is unknown.
Symptoms in people infected by H5N1 are similar, but more severe than typical, seasonal flu. Viral pneumonia and acute respiratory distress has been the primary cause of death.
WHO, CDC, NIAID, Chotpitayasunondh T, et al. Human disease from influenza A (H5N1), Thailand, 2004. Emerg Infect Dis, 2005; 11(2):201-9