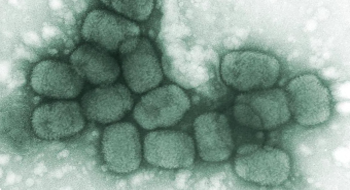

Smallpox is a deadly and highly contagious disease caused by Variola major, a double-stranded DNA orthopox virus. It has been a major cause of death throughout history, killing more than 500 million people in the 20th century. For comparison, the current population of the United States is a little over 300 million. Transmission occurs mainly through the inhalation of respiratory droplets (formed by coughing and sneezing) from infected individuals. It can also spread through fomites, which are scab contaminated materials such as bedding and clothing. The ordinary presentation of smallpox has a fatality rate of approximately 30% among unvaccinated and untreated individuals. Because smallpox only infects humans and cannot survive for more than a few months outside its host under the most optimal conditions, it was a good candidate for disease eradication by the World Health Organization (WHO). The WHO’s 12 year global containment and vaccination program was successful, and smallpox was declared as eradicated from the global population in 1979. Stocks of the virus are kept by the United States and Russia for research purposes.
Variola major is considered an effective bioweapon for a number of reasons. First, it is highly contagious; a single uncontrolled case would likely infect 3-6 more people, exponentially spreading the disease. It also has a low infectious dose and a relatively high fatality rate. In addition, V. major can be stable for hours as an aerosol (over 24 hours in optimal environmental conditions) and can be produced and stored in large quantities. The majority of the global population is unvaccinated against smallpox, making. The Soviet Union produced tons of weaponized Variola major per year during the Cold War, in violation of the 1975 Biological Weapons Convention. With the fall of the Soviet Union in 1991 and the disarray that followed, stocks of smallpox may exist outside of the designated research facility in Russia, and some may have been transferred to other state bioweapons programs.
Virulence factors make an organism dangerous. There are two known virulence factors in Variola major that help the virus evade the human immune system. The first is a protein called SPICE (Smallpox Inhibitor of Complement Enzymes), which helps the virus evade detection and destruction by inactivating key proteins in a part of the immune system known as the complement system. The second known virulence factor, CKBP-II (secreted Chemokine-Binding Protein, type 2), blocks signals that call for more immune cells and promote inflammation at the site of infection. The Vaccinia virus, used for smallpox vaccinations, has proteins that are similar to both SPICE and CKBP-II, but are much less potent. This supports the idea that SPICE and CKBP-II are key factors for Variola major‘s virulence.
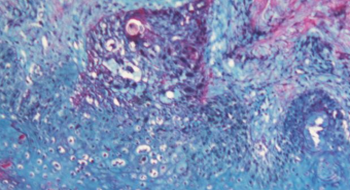
Severe flu-like symptoms, including headache, high fever, malaise and fatigue, begin approximately 12 days after exposure to Variola major. 1-4 days later an enantham rash appears on the infected individual’s mucus membranes (the inside of the mouth, nose and throat). The infected individual is highly contagious at this stage and for the following week. 24 hours later, an external rash, the exantham, appears all over the body, with higher concentrations of lesions on the face, arms and legs. The classic pox lesions are firm, umbilicated (indented in the center), and progress together through the stages of lesion development (maculopapular rash, vesicles, pustules, scabs, scars). After 8-9 days of the rash, the smallpox pustules begin to scab over and fall off. Individuals are less contagious at this stage, but continue to be contagious until the last scab has fallen off. Permanent scars, blindness, and arthritis can result from the infection. Variola minor causes alastrim, a milder form of smallpox with a fatality rate of < 1%. Ordinary smallpox, caused by Variola major, has a fatality rate of 30%. In 2% to 6% of smallpox infections, the lesions are classified as either hemorrhagic, characterized by bleeding sores, or flat, where the lesions are soft and flat. The mortality rates for these types of infections are over 95%.
Typically, the Variola virus first infects the lining of the throat, where it is taken-up by immune cells and transferred to the local lymph nodes. It replicates for 3-4 days and enters the blood stream in a state called viremia, which helps the virus spread to the spleen, bone marrow, and additional lymph nodes. There, the virus continues to replicate, destroying cells in the process. Throughout replication, Variola major produces virulence factors that disrupt the normal functioning of the human immune system. Around the 8th day, the virus re-enters the blood stream and begins to localize in the small blood vessels near the surface of the skin and mucous membranes. At this time, patients may begin to experience the initial fever and other prodromal symptoms. The virus continues to replicate near the skin surface, spreading and killing cells. This replication and cell death near the skin surface causes the smallpox irritations and lesions.
Treatment remains largely experimental. Injection with Vaccinia Immunoglobulin (VIG), antibodies produced against the vaccinia virus, may help alleviate some symptoms. The antiviral medication cidofovir may be used in emergency situations, and ST-246®, a new and promising smallpox antiviral, is currently undergoing phase I clinical trials. In addition to other supportive care, antibiotics are given to reduce potential secondary bacterial infections. Vaccination after exposure to smallpox is protective if given sufficiently early.
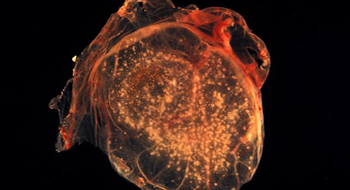
In 1796, Edward Jenner developed the first vaccine against smallpox using material that contained the cowpox virus. The modern smallpox vaccine contains Vaccinia virus, (unrelated to the cowpox virus) and is administered by small jabs to the skin with a bifurcated (two- pronged) needle. Routine vaccination in the United States stopped in 1972 because the risks of vaccine complications outweighed the risk of a smallpox infection. A smallpox-like lesion will develop at the site of inoculation and should not be touched until the scab falls off. This is because the virus can be spread to different locations on the body (autoinnoculation) or to others. Other possible vaccine complications include: generalized and progressive vaccinia, where lesions erupt in multiple locations on the body due to systemic spread of the vaccinia virus; eczema vaccinatum, a more serious complication that occurs in individuals with eczema or related skin problems; and post-vaccinial encephalitis (inflammation of the brain), a rare (1:1,000,000), but frequently fatal complication.
Dembek, ZF [Senior Editor] (2007). Smallpox and Related Orthopoxviruses, Chapter 11, Medical Aspects of Chemical and Biological Warfare. Publisher: Department of Defense, Office of The Surgeon General, US Army, Borden Institute. 2007: 672 p.; ill http://www.bordeninstitute.army.mil/published_volumes/biological_warfare/biological.html
Henderson, D.A. et al (1999). Smallpox as a Biological Weapon. JAMA. 1999; Vol 281, No. 22: 2127-2173.
Dunlop, L.R., et al. (2003) Variola virus immune evasion proteins, Microbes and Infection, Volume 5, Issue 11, September 2003, Pages 1049-1056, ISSN 1286-4579, DOI: 10.1016/S1286-4579(03)00194-1. (http://www.sciencedirect.com/science/article/B6VPN-494GKKK-1/2/297829a2b0ff6edc278a4b80486df725)
Raymond Gani & Steve Leach (2001). Transmission potential of smallpox in contemporary populations. Nature 414, 748-751 (13 December 2001) | doi:10.1038/414748a; Received 8 October 2001; Accepted 5 November 2001